To correct anatomical problems associated with infertility and pregnancy loss your doctor may prescribe a laparoscopy or hysteroscopy
Laparoscopy and hysteroscopy are two of the most common minimally invasive gynecological surgical procedures to either diagnose a woman’s infertility or correct problems that cause infertility and miscarriage.
Minimally invasive techniques require no or only a few small incisions, rather than one large incision. Some of the procedures can be done on an outpatient basis, others may require a short hospital stay of one to two nights.
The gynecological surgeons at Fertility Answers are leaders in minimally invasive options to treat gynecologic conditions. Our physicians have specialized training and extensive expertise in techniques and technology for minimally invasive gynecologic procedures. Our team can treat complex conditions, such as large fibroids and advanced endometriosis, that other centers cannot.
Benefits of gynecologic minimally invasive surgery
Minimally invasive techniques offer a safer and effective alternative to traditional open surgery by avoiding a large abdominal incision. With minimally invasive gynecologic surgery, our patients can have:
- Smaller incisions
- Less blood loss
- Less pain
- Shorter hospital stays
- Faster recovery and return to daily activities
- Reduced scar tissue
- Less risk of infection or other complications
A laparoscopy allows the physician to have direct visualization of the ovaries, tubes and uterus
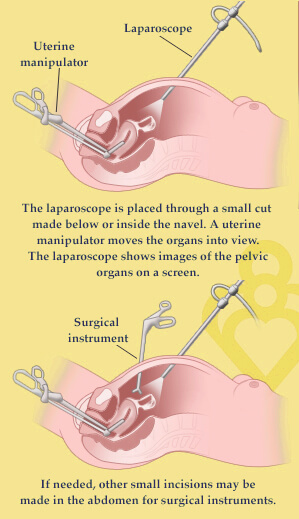 Laparoscopy, also known as minimally invasive surgery, is direct visualization of the peritoneal cavity, ovaries, outside of the tubes and uterus by using a laparoscope.
Laparoscopy, also known as minimally invasive surgery, is direct visualization of the peritoneal cavity, ovaries, outside of the tubes and uterus by using a laparoscope.
An abdominal laparoscopy can be done to check the abdomen and its organs for uterine fibroids and other growths, abnormal bleeding, abdominal pain, ovarian cysts, and to check the tubes for visible blockages. A laparoscopy is often done when the results of a physical exam or other tests are not clear. Laparoscopy can also be used to treat endometriosis.
Laparoscopy often requires only a few 0.5 cm incisions through the abdominal wall. The surgeon inserts a laparoscope into the abdomen through these small incisions to view and make surgical corrections to the pelvic structures involved. The laparoscope is an instrument somewhat like a miniature telescope with a fiber optic system, which brings light into the abdomen. It is about as big around as a fountain pen and twice as long.
An instrument to move the uterus during surgery will be placed in the vagina. Carbon dioxide (CO2) is put into the abdomen through a special needle that is inserted just below the navel. This gas helps to separate the organs inside the abdominal cavity, making it easier for the physician to see the reproductive organs during laparoscopy. The gas is removed at the end of the procedure.
Laparoscopy is more invasive than a hysteroscopy, but a less-invasive procedure than open abdominal surgery and allows for a quicker recovery with a lower risk of adhesion (scar tissue) formation. Most patients go home the same day as the procedure and return to work 3-4 days later.
Hysteroscopy uses no incisions at all
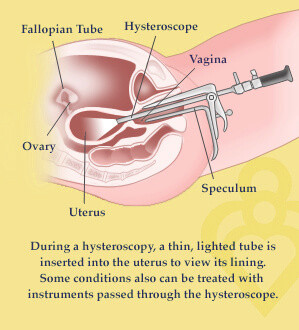 A hysteroscopy is used to diagnose the cause of infertility or repeated miscarriages, biopsy endometrial tissue, and to examine and remove uterine scarring, polyps, or small fibroids.
A hysteroscopy is used to diagnose the cause of infertility or repeated miscarriages, biopsy endometrial tissue, and to examine and remove uterine scarring, polyps, or small fibroids.
During an operative hysteroscopy, a small hysteroscope is inserted through the cervix and advanced into the uterine cavity with the patient asleep under general anesthesia. Like a laparoscope, the hysteroscope is an instrument somewhat like a miniature telescope with a fiber optic system, which brings light into the uterus. This procedure allows for direct views of the uterine cavity and permits the physician to surgically correct the abnormality.
Your Fertility Answers provider may do your hysteroscopy in our office surgical suite or in an outpatient center. You may have local or no anesthesia. Procedures that are more complex may be done in the operating room under local, regional, or general anesthesia. Patients generally go home the same day as the procedure and can often return to work the next day.


